Error message

Jivanta Schottli, Assistant Professor in Indian Politics and Foreign Policy at Dublin City University and Director of the Ireland India Institute, asks what needs to be done in India’s hour of need and explores the challenges India faces on its way forward through an unprecedented second wave of the COVID-19 pandemic.
India struggled with an unprecedented second wave of the COVID-19 pandemic. At its height, more than 400,000 new coronavirus cases were being reported daily. In many countries, the second wave was more virulent than the first, mirroring what happened in the fall of 1918, the second and deadliest phase of the Spanish influenza pandemic. Foreign aid poured into India, but the main challenge is to enable and fast-track partnerships and to ramp up vaccine production. Facing an acute situation at home, the Government of India suspended vaccine exports in late March. This was a major blow to countries who had either received doses as part of India’s vaccine diplomacy, or had placed orders with India’s Serum Institute, the world’s largest vaccine producer. In total, India shipped 64 million doses of vaccines to 85 countries. China has stepped in to fill the gap, further cementing its status as the world’s largest vaccine exporter.
Since the pandemic began last year, India reported more than 23 million cases and more than 250,000 deaths. In the first seven days of May, India recorded 2.7 million cases and over 25,700 deaths. Earlier in March, cases began to skyrocket in India’s richest state Maharashtra, home to the country’s financial capital Mumbai, a city with an estimated population of 12.5 million. During March, Maharashtra accounted for nearly 70% of the national caseload. Throughout April, a more potent variant of the virus accelerated infection rates and spread across the country. At the time of writing, not only Delhi but states to the north, west, and south experienced shocking, heart-wrenching scenes of suffering spurred on by a lack of oxygen supplies, intensive care units, and hospital beds. Although authorities did not announce a national lockdown, restrictions ranging from complete lockdowns to partial curfews were put in place across the country’s 28 states and eight union territories.
The question of why India was caught off guard after weathering the first wave of the pandemic, which peaked in September 2020, is a point of heated discussion. After a long and economically painful nationwide lockdown from March to June 2020, the country’s reopening began to release pent-up demand and allowed citizens a chance to recover lost livelihoods. A feeling of normalcy crept into daily life, a false sense of security, with restrictions being eased and large social gatherings allowed to take place. Mass religious congregations were permitted, as were massive election rallies in four states. Politicians, policymakers, and parts of the media believed the worst was over and the virus had been defeated.
The extent to which the central and state governments should be blamed for not being more prepared, failing to heed warnings, or not having contingencies in place for an imminent second wave is the subject for another paper. Here, the question is, what needs to be done in India’s hour of need? The world responded to India’s call for aid. Essential medical supplies arrived from countries that acknowledged the help given by India to them earlier during their moments of crisis in the pandemic. At the same time,
there were complaints about delays in distributing critical supplies, the lack of transparency, and unclear procurement processes.
Beyond the immediate need for and distribution of critical and life-saving medical supplies across the country is the urgent need to vaccinate. The rollout of the country’s own vaccination program has been slow. India’s vaccination program had an ambitious launch on January 16th using two locally manufactured vaccines, the Oxford-AstraZeneca “Covishield” and the domestic Bharat Biotech “Covaxin.” Vaccine uptake was slower than expected, encumbered by the challenge of reaching vast and far-flung populations. A lack of interest from the public, amidst other more pressing health priorities, contributed to low inoculation rates. India has administered more than 160 million doses, a high absolute number but only enough to vaccinate a little more than 11% of India’s population.
On May 1st, India opened Covid-19 vaccinations to all adults. The federal government designated states as solely responsible for procuring and administering vaccines for the 18-44 age group. This abdication of responsibility amidst a critical shortage of doses frayed relations between central and state governments. Rising tensions were further exacerbated by raw material bottlenecks in the global supply chain, confusion over pricing, and unclear procurement procedures.
On May 5th, another crucial development occurred. President Joe Biden’s administration announced support for a global waiver on patent protections for Covid-19 vaccines, to be negotiated at the World Trade Organization (WTO). The move was welcomed by many – indeed, India and South Africa have been leading calls in the WTO to temporarily remove intellectual property protections on Covid-19 vaccines since September 2020. It has also been met with surprise and criticism by pharmaceutical giants and their host countries.
The negotiation of a patent waiver will take time. Many analysts believe the announcement will push industry and governments towards more licensing partnerships between vaccine creators and manufacturers. Pharma giants like Pfizer, which initially showed an interest in manufacturing in India but only on terms of their choosing, may re-consider entering into an arrangement with a local partner.
At this time of crisis, the Government of India is exploring ways to boost vaccine production at home through domestic technology transfers while examining options to urgently ramp up supplies through collaborations with foreign entities. It is also a moment of reckoning for the Quadrilateral Security Dialogue (Quad) members - United States, Japan, Australia, and India. Earlier this year, at its first leaders’ meeting, health security was a crucial element in the summit’s joint statement. A Quad Vaccine Partnership was promised, with a specific focus on expanding manufacturing capacity in India. India’s hour of need is also a test of the extent to which the Quad, which includes two of the world’s leading economies, is willing and able to strive towards “a region that is free, open, inclusive, healthy, anchored by democratic values, and unconstrained by coercion.1”
1 Quadrilateral Security Dialogue. “United States Quad Leaders’ Joint Statement: ‘The Spirit of the Quad.’” March 12, 2021. https://www.whitehouse.gov/briefing-room/statements-releases/2021/03/12/quad-leaders-joint-statement-the-spirit-of-the-quad/#:~:text=1.,free%20and%20open%20Indo%2DPacific.
Jivanta Schottli, Assistant Professor in Indian Politics and Foreign Policy at Dublin City University and Director of the Ireland India Institute, asks what needs to be done in India’s hour of need and explores the challenges India faces on its way forward through an unprecedented second wave of the COVID-19 pandemic.
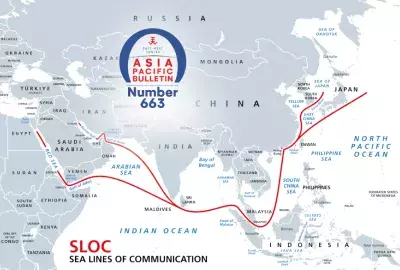
India struggled with an unprecedented second wave of the COVID-19 pandemic. At its height, more than 400,000 new coronavirus cases were being reported daily. In many countries, the second wave was more virulent than the first, mirroring what happened in the fall of 1918, the second and deadliest phase of the Spanish influenza pandemic. Foreign aid poured into India, but the main challenge is to enable and fast-track partnerships and to ramp up vaccine production. Facing an acute situation at home, the Government of India suspended vaccine exports in late March. This was a major blow to countries who had either received doses as part of India’s vaccine diplomacy, or had placed orders with India’s Serum Institute, the world’s largest vaccine producer. In total, India shipped 64 million doses of vaccines to 85 countries. China has stepped in to fill the gap, further cementing its status as the world’s largest vaccine exporter.
Since the pandemic began last year, India reported more than 23 million cases and more than 250,000 deaths. In the first seven days of May, India recorded 2.7 million cases and over 25,700 deaths. Earlier in March, cases began to skyrocket in India’s richest state Maharashtra, home to the country’s financial capital Mumbai, a city with an estimated population of 12.5 million. During March, Maharashtra accounted for nearly 70% of the national caseload. Throughout April, a more potent variant of the virus accelerated infection rates and spread across the country. At the time of writing, not only Delhi but states to the north, west, and south experienced shocking, heart-wrenching scenes of suffering spurred on by a lack of oxygen supplies, intensive care units, and hospital beds. Although authorities did not announce a national lockdown, restrictions ranging from complete lockdowns to partial curfews were put in place across the country’s 28 states and eight union territories.
The question of why India was caught off guard after weathering the first wave of the pandemic, which peaked in September 2020, is a point of heated discussion. After a long and economically painful nationwide lockdown from March to June 2020, the country’s reopening began to release pent-up demand and allowed citizens a chance to recover lost livelihoods. A feeling of normalcy crept into daily life, a false sense of security, with restrictions being eased and large social gatherings allowed to take place. Mass religious congregations were permitted, as were massive election rallies in four states. Politicians, policymakers, and parts of the media believed the worst was over and the virus had been defeated.
The extent to which the central and state governments should be blamed for not being more prepared, failing to heed warnings, or not having contingencies in place for an imminent second wave is the subject for another paper. Here, the question is, what needs to be done in India’s hour of need? The world responded to India’s call for aid. Essential medical supplies arrived from countries that acknowledged the help given by India to them earlier during their moments of crisis in the pandemic. At the same time,
there were complaints about delays in distributing critical supplies, the lack of transparency, and unclear procurement processes.
Beyond the immediate need for and distribution of critical and life-saving medical supplies across the country is the urgent need to vaccinate. The rollout of the country’s own vaccination program has been slow. India’s vaccination program had an ambitious launch on January 16th using two locally manufactured vaccines, the Oxford-AstraZeneca “Covishield” and the domestic Bharat Biotech “Covaxin.” Vaccine uptake was slower than expected, encumbered by the challenge of reaching vast and far-flung populations. A lack of interest from the public, amidst other more pressing health priorities, contributed to low inoculation rates. India has administered more than 160 million doses, a high absolute number but only enough to vaccinate a little more than 11% of India’s population.
On May 1st, India opened Covid-19 vaccinations to all adults. The federal government designated states as solely responsible for procuring and administering vaccines for the 18-44 age group. This abdication of responsibility amidst a critical shortage of doses frayed relations between central and state governments. Rising tensions were further exacerbated by raw material bottlenecks in the global supply chain, confusion over pricing, and unclear procurement procedures.
On May 5th, another crucial development occurred. President Joe Biden’s administration announced support for a global waiver on patent protections for Covid-19 vaccines, to be negotiated at the World Trade Organization (WTO). The move was welcomed by many – indeed, India and South Africa have been leading calls in the WTO to temporarily remove intellectual property protections on Covid-19 vaccines since September 2020. It has also been met with surprise and criticism by pharmaceutical giants and their host countries.
The negotiation of a patent waiver will take time. Many analysts believe the announcement will push industry and governments towards more licensing partnerships between vaccine creators and manufacturers. Pharma giants like Pfizer, which initially showed an interest in manufacturing in India but only on terms of their choosing, may re-consider entering into an arrangement with a local partner.
At this time of crisis, the Government of India is exploring ways to boost vaccine production at home through domestic technology transfers while examining options to urgently ramp up supplies through collaborations with foreign entities. It is also a moment of reckoning for the Quadrilateral Security Dialogue (Quad) members - United States, Japan, Australia, and India. Earlier this year, at its first leaders’ meeting, health security was a crucial element in the summit’s joint statement. A Quad Vaccine Partnership was promised, with a specific focus on expanding manufacturing capacity in India. India’s hour of need is also a test of the extent to which the Quad, which includes two of the world’s leading economies, is willing and able to strive towards “a region that is free, open, inclusive, healthy, anchored by democratic values, and unconstrained by coercion.1”
1 Quadrilateral Security Dialogue. “United States Quad Leaders’ Joint Statement: ‘The Spirit of the Quad.’” March 12, 2021. https://www.whitehouse.gov/briefing-room/statements-releases/2021/03/12/quad-leaders-joint-statement-the-spirit-of-the-quad/#:~:text=1.,free%20and%20open%20Indo%2DPacific.