Error message


Neal A. Palafox, MD, MPH, Professor, Department of Family Medicine and Community Health, John A. Burns School of Medicine, University of Hawaii, & Wilfred C. Alik, MD, Clinic Chief for the Kaiser Permanente Medical Center in Hilo, HI, Co-Founder of the Micronesian Health Advisory Coalition, and Chairman of Marshallese COVID-19 Task Force, "articulate a disparate range of pandemic experiences across Pacific Island countries and territories (PICTs), in terms of COVID 19 community transmission, cases, mortality, and vaccination rates."
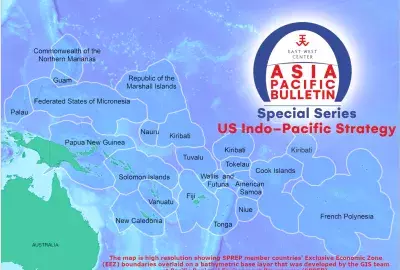
This brief compares COVID-19 data across Pacific countries through the first week of June 2022. Data is drawn from regional reports from the World Health Organization (WHO) , which has monitored the pandemic in Oceania since early March 2020, and situation reports on US-affiliated Pacific Islands compiled by the Pacific Islanders Health Organization Associations (PIHOA). These reports articulate a disparate range of pandemic experiences across Pacific Island countries and territories (PICTs), in terms of COVID 19 community transmission, cases, mortality, and vaccination rates.
COVID 19 made its Western Pacific debut in 2020 as winter gave way to spring. In February of that year, 712 cases developed amongst the crew and passengers aboard the Diamond Princess cruise ship, resulting in 14 deaths. During the following month, the USS Theodore Roosevelt aircraft carrier, was forced dockside in Guam due to a COVID-19 outbreak among its crew, which resulted in two-thirds of the nearly 5000 sailors on board contracting the virus and one death. By November, French Polynesia and Guam recorded over 12,500 cases with 62 deaths and 6,400 cases with 101 deaths respectively. Some Pacific countries remained without COVID-19 community transmission as they closed their borders to international travel. As a high priority every Pacific Island country moved quickly to acquire ventilators, personal protective equipment (PPE), in-country COVID-19 testing capacity, and vaccinations. Across the region, a substantial portion of the limited pool of government and health workers were deployed in COVID-19 responses.
Transmission rates in the Pacific varied across World Bank income designations for sovereign nations and territories, low- or middle-income (LMI), upper middle-income (UMI) and High-Income. Guam and French Polynesia, High-Income US and French territories respectively, suffered the highest rates of community transmission and mortality early in the Pandemic and through the middle of the second COVID-19 Delta wave. Conversely, the Republic of the Marshall Islands (RMI), UMIC; American Samoa, UMIC; Republic of Palau, HIC; and the Federated States of Micronesia, LMIC, had no community transmission and deaths through the first 18 months of the global pandemic. However, over the last 7 months, American Samoa and the Republic of Palau have observed a notable increase in community transmission and COVID-19 deaths. The PICTs without any COVID-19 community transmission and mortality in Oceania are Niue, Tuvalu, RMI, Micronesia, and Nauru, three of these five covid free jurisdictions are designated as LMI. Transmission rates were not exacerbated in locations with larger populations. The Pacific countries with the largest populations, Solomon Islands, Fiji, and Papua New Guinea, have community transmission and mortality rates significantly less than Guam and French Polynesia although their populations are three times greater or more.
Comparing vaccination rates in the Northern Pacific, PICTs that have completed-vaccination rates of greater than 85%, are Guam, the Commonwealth of the Northern Mariana Islands, Palau, and American Samoa. These locations were still associated with significant COVID-19 community transmission rates and moderate mortality rates. However, more granular data on the timeline for vaccination deployment is needed to understand the relative benefit of vaccination in countries and territories. FSM and RMI had complete-vaccination rates of between 56% to 75% and had no COVID-19 community transmission or deaths.
Throughout the region, mainstay public health measures to prevent and control COVID-19, such as COVID-19 health literacy programs, masking policies, bactericidal solutions, social distancing, and isolation were in place within three months after the onset of the Pandemic. Technological COVID-19 control measures, such as protective equipment, testing, sufficient quantities of hospital ventilators, were made available to most Pacific nations by November 2020, 7 months into the Pacific Pandemic. Adequate vaccines were available within 11-14 months. Strategic and timely deployment of the various technologies varied with country health workforce capacity, community preparedness, and policy maker perspectives.
Each PICT handled the COVID-19 outbreak in a different way. At the onset of the pandemic RMI, American Samoa, the Republic of Palau, and FSM closed their borders. The border control was strict, and many of the citizens of Palau, RMI, and FSM could not return to their home islands for the first 18 months of the pandemic. This was followed by tightly controlled repatriation efforts which began between 10 to 14 months after the onset of the pandemic. The initial quarantine policies of RMI and FSM required 14 days quarantine and negative testing before departing and another 14 days upon arrival. In contrast, French Polynesia and Guam maintained open borders with testing requirements for entry.
What are the metrics of success for each country or territory within Oceania with respect to COVID-19? Is success measured by low or nonexistent COVID-19 community transmission and death rates, high vaccination rates, or adequate testing and treatment facilities? What are the most effective COVID-19 protective and risk reduction measures for the Pacific? Apparently, being a high-income jurisdiction or a territory of a large industrial nation does not ensure low transmission and death rates. In fact, one could argue that high income status or being a territory of a larger industrialized nation is predictive of worse COVID-19 outcomes. Having a comparatively larger population did not seem to put jurisdictions at a greater risk for poor COVID-19 outcomes either, as some of the Pacific Nations with the highest community transmission and death rates had neither the largest nor the smallest populations.
The COVID-19 pandemic is not over, and the consequences of high infection rates and high hospitalization rates will be the proliferation of COVID-19 long hauler’s illnesses. There continues to be a health crisis globally and in the Pacific. Essential health services, education, social services, and economic growth has been paused or completely stopped during these last two years. For each Pacific jurisdiction, health policy makers and community leaders should give pause and reflect on what they learned, how they could have done better, and how to proceed in an ongoing pandemic.
Perhaps, PICTs demonstrate how the COVID-19 pandemic can be handled, with or without technologically advanced health systems, deep coffers, political independence, or a large population. The data clearly indicates that health policy and community mobility in each jurisdiction was the major instrument of COVID-19 prevention and control—not technology. This is an opportunity for the region to realize that significant COVID-19 control can be achieved anywhere. Understanding COVID-19 outcomes in terms of health policy and community mobilization is essential as Pacific Island nations and territories continue to navigate through this global pandemic.

Neal A. Palafox, MD, MPH, Professor, Department of Family Medicine and Community Health, John A. Burns School of Medicine, University of Hawaii, & Wilfred C. Alik, MD, Clinic Chief for the Kaiser Permanente Medical Center in Hilo, HI, Co-Founder of the Micronesian Health Advisory Coalition, and Chairman of Marshallese COVID-19 Task Force, "articulate a disparate range of pandemic experiences across Pacific Island countries and territories (PICTs), in terms of COVID 19 community transmission, cases, mortality, and vaccination rates."
This brief compares COVID-19 data across Pacific countries through the first week of June 2022. Data is drawn from regional reports from the World Health Organization (WHO) , which has monitored the pandemic in Oceania since early March 2020, and situation reports on US-affiliated Pacific Islands compiled by the Pacific Islanders Health Organization Associations (PIHOA). These reports articulate a disparate range of pandemic experiences across Pacific Island countries and territories (PICTs), in terms of COVID 19 community transmission, cases, mortality, and vaccination rates.
COVID 19 made its Western Pacific debut in 2020 as winter gave way to spring. In February of that year, 712 cases developed amongst the crew and passengers aboard the Diamond Princess cruise ship, resulting in 14 deaths. During the following month, the USS Theodore Roosevelt aircraft carrier, was forced dockside in Guam due to a COVID-19 outbreak among its crew, which resulted in two-thirds of the nearly 5000 sailors on board contracting the virus and one death. By November, French Polynesia and Guam recorded over 12,500 cases with 62 deaths and 6,400 cases with 101 deaths respectively. Some Pacific countries remained without COVID-19 community transmission as they closed their borders to international travel. As a high priority every Pacific Island country moved quickly to acquire ventilators, personal protective equipment (PPE), in-country COVID-19 testing capacity, and vaccinations. Across the region, a substantial portion of the limited pool of government and health workers were deployed in COVID-19 responses.
Transmission rates in the Pacific varied across World Bank income designations for sovereign nations and territories, low- or middle-income (LMI), upper middle-income (UMI) and High-Income. Guam and French Polynesia, High-Income US and French territories respectively, suffered the highest rates of community transmission and mortality early in the Pandemic and through the middle of the second COVID-19 Delta wave. Conversely, the Republic of the Marshall Islands (RMI), UMIC; American Samoa, UMIC; Republic of Palau, HIC; and the Federated States of Micronesia, LMIC, had no community transmission and deaths through the first 18 months of the global pandemic. However, over the last 7 months, American Samoa and the Republic of Palau have observed a notable increase in community transmission and COVID-19 deaths. The PICTs without any COVID-19 community transmission and mortality in Oceania are Niue, Tuvalu, RMI, Micronesia, and Nauru, three of these five covid free jurisdictions are designated as LMI. Transmission rates were not exacerbated in locations with larger populations. The Pacific countries with the largest populations, Solomon Islands, Fiji, and Papua New Guinea, have community transmission and mortality rates significantly less than Guam and French Polynesia although their populations are three times greater or more.
Comparing vaccination rates in the Northern Pacific, PICTs that have completed-vaccination rates of greater than 85%, are Guam, the Commonwealth of the Northern Mariana Islands, Palau, and American Samoa. These locations were still associated with significant COVID-19 community transmission rates and moderate mortality rates. However, more granular data on the timeline for vaccination deployment is needed to understand the relative benefit of vaccination in countries and territories. FSM and RMI had complete-vaccination rates of between 56% to 75% and had no COVID-19 community transmission or deaths.
Throughout the region, mainstay public health measures to prevent and control COVID-19, such as COVID-19 health literacy programs, masking policies, bactericidal solutions, social distancing, and isolation were in place within three months after the onset of the Pandemic. Technological COVID-19 control measures, such as protective equipment, testing, sufficient quantities of hospital ventilators, were made available to most Pacific nations by November 2020, 7 months into the Pacific Pandemic. Adequate vaccines were available within 11-14 months. Strategic and timely deployment of the various technologies varied with country health workforce capacity, community preparedness, and policy maker perspectives.
Each PICT handled the COVID-19 outbreak in a different way. At the onset of the pandemic RMI, American Samoa, the Republic of Palau, and FSM closed their borders. The border control was strict, and many of the citizens of Palau, RMI, and FSM could not return to their home islands for the first 18 months of the pandemic. This was followed by tightly controlled repatriation efforts which began between 10 to 14 months after the onset of the pandemic. The initial quarantine policies of RMI and FSM required 14 days quarantine and negative testing before departing and another 14 days upon arrival. In contrast, French Polynesia and Guam maintained open borders with testing requirements for entry.
What are the metrics of success for each country or territory within Oceania with respect to COVID-19? Is success measured by low or nonexistent COVID-19 community transmission and death rates, high vaccination rates, or adequate testing and treatment facilities? What are the most effective COVID-19 protective and risk reduction measures for the Pacific? Apparently, being a high-income jurisdiction or a territory of a large industrial nation does not ensure low transmission and death rates. In fact, one could argue that high income status or being a territory of a larger industrialized nation is predictive of worse COVID-19 outcomes. Having a comparatively larger population did not seem to put jurisdictions at a greater risk for poor COVID-19 outcomes either, as some of the Pacific Nations with the highest community transmission and death rates had neither the largest nor the smallest populations.
The COVID-19 pandemic is not over, and the consequences of high infection rates and high hospitalization rates will be the proliferation of COVID-19 long hauler’s illnesses. There continues to be a health crisis globally and in the Pacific. Essential health services, education, social services, and economic growth has been paused or completely stopped during these last two years. For each Pacific jurisdiction, health policy makers and community leaders should give pause and reflect on what they learned, how they could have done better, and how to proceed in an ongoing pandemic.
Perhaps, PICTs demonstrate how the COVID-19 pandemic can be handled, with or without technologically advanced health systems, deep coffers, political independence, or a large population. The data clearly indicates that health policy and community mobility in each jurisdiction was the major instrument of COVID-19 prevention and control—not technology. This is an opportunity for the region to realize that significant COVID-19 control can be achieved anywhere. Understanding COVID-19 outcomes in terms of health policy and community mobilization is essential as Pacific Island nations and territories continue to navigate through this global pandemic.